Advances in Chimeric Antigen Receptor (CAR) T Cell Therapy for Multiple Myeloma
Advances in Chimeric Antigen Receptor (CAR) T Cell Therapy for Multiple Myeloma
Multiple myeloma (MM) is a malignant plasma cell disease and the second most common hematological malignancy. Currently, there is no curative treatment available. Despite the emergence of new drugs, drug resistance and relapse in MM remain the focus of current research, and better therapies are urgently needed. Chimeric antigen receptor T-cell (CAR-T) therapy is a novel treatment approach that has shown promising therapeutic prospects in the treatment of MM, bringing hope for a cure. This article describes the recent progress of CAR-T therapy in the treatment of MM, including its clinical efficacy, safety, and accessibility, in order to further optimize treatment strategies.
Keywords
Multiple myeloma; Chimeric antigen receptor T cells; Target selection; Adverse reactions
Multiple myeloma (MM) is a clonal plasma cell disorder characterized by the uncontrolled proliferation of clonal plasma cells in the bone marrow and impaired apoptosis, resulting in the production of abnormal amounts of monoclonal immunoglobulins and subsequent end-organ dysfunction. MM is the second most common hematological malignancy, accounting for approximately 1% of all cancers and 13% of hematological malignancies. Currently, it is incurable, and the relapse rate is extremely high. Although the use of proteasome inhibitors, immunomodulatory drugs, monoclonal antibodies, and hematopoietic stem cell transplantation has improved the response rate, depth of response, and survival time in MM patients, drug resistance or relapse remains a clinical challenge, necessitating the exploration of new treatment modalities.
Chimeric antigen receptor T-cell (CAR-T) therapy is a novel treatment approach that has shown promising therapeutic prospects in the treatment of MM. This article describes the recent progress of CAR-T therapy, including target selection and application, optimization of CAR-T cells, improvement of production processes, and cost reduction, with the aim of facilitating the translation of clinical research into survival benefits for patients.
1. Overview of CAR-T Cell Therapy
1.1) Principle and Mechanism of CAR-T Cell Therapy
CAR-T cell therapy is a form of cellular immunotherapy that involves genetically modifying T cells to express chimeric antigen receptors (CARs) that can directly recognize and bind to specific antigens on the surface of tumor cells, leading to T cell activation, proliferation, and targeted killing of tumor cells.
CAR-T cells combine the antigen specificity with the cytotoxic potency of T cells. The CAR is the key technological component, typically composed of an extracellular antigen-binding domain derived from a single-chain variable fragment (scFv) of a monoclonal antibody, and intracellular signaling domains, usually including the CD3ζ domain from the T cell receptor (TCR) complex and one or more co-stimulatory domains such as CD28 or 4-1BB. Upon binding to the specific antigen on tumor cells, the signaling domains of the CAR activate and promote the proliferation of CAR-T cells, which subsequently secrete cytokines or directly kill the targeted tumor cells. The concept of CARs was first proposed by Gross, Waks, and Eshhar in the late 1980s, and CARs have undergone several iterations and updates since then.
(1) First-generation CARs: Lack co-stimulatory domains and rely solely on the CD3ζ signaling domain to induce T cell activation. They possess antigen-specific cytotoxicity against tumor cells but have limited T cell proliferation capabilities.
(2) Second-generation CARs: Incorporate one co-stimulatory domain (e.g., CD27, CD28, CD134, or 4-1BB), improving the in vivo characteristics of CAR-T cells. For example, the inclusion of the 4-1BB co-stimulatory domain enhances T cell proliferation and persistence.
(3) Third-generation CARs: Contain two co-stimulatory domains, further enhancing intracellular signaling activity and conferring superior in vivo expansion and persistence of CAR-T cells.
(4) Fourth-generation CARs: Ushered in the era of precision cancer therapy. By incorporating additional genetic modifications (e.g., suicide genes or drug-inducible genes) into the CAR structure, these CARs aim to enhance anti-tumor effects or reduce cellular toxicity through combinatorial approaches.
(5) Fifth-generation CARs, also known as universal CAR-T cells (UCAR-T): Derived from healthy donor T cells that have undergone gene editing to disrupt specific genes, UCAR-T cells offer the advantage of not requiring patient-derived T cells and can be produced in bulk and stored for off-the-shelf use.
Additionally, some novel cell therapies based on CAR technology are under development, including CAR-NK cells, CAR-macrophages, and CAR-regulatory T cells. These innovative cell therapies combine CAR technology with gene engineering approaches to modify the cellular genome, aiming to improve their performance compared to traditional CAR-T cells, such as better targeting of solid tumors or enhanced persistence in the tumor microenvironment. Currently, second-generation CAR-T products dominate the approved CAR-T market, while fourth-generation CAR-T products are actively being developed and hold promise for clinical translation. Fifth-generation UCAR-T cells also offer exciting prospects.
1.2) Application of CAR-T Cell Therapy in Hematological Malignancies
CAR-T cell therapy has been applied to the treatment of various hematological malignancies. To date, nine CAR-T products have been approved globally, with three approved by the National Medical Products Administration (NMPA) in China and six approved by the U.S. Food and Drug Administration (FDA), all of which are indicated for the treatment of hematological malignancies.
Sun et al. reported that 73% of CAR-T clinical trials in China were focused on hematological malignancies, and similar trends have been observed in other countries. CAR-T cell therapy has demonstrated significant clinical efficacy in the treatment of hematological malignancies, including diffuse large B-cell lymphoma (DLBCL), acute B-lymphoblastic leukemia (B-ALL), and multiple myeloma (MM).
In the treatment of DLBCL, CD19-targeted CAR-T cell therapy has shown promising results, with overall response rates ranging from 52% to 82% and 40% to 54% of patients achieving durable long-term remission. Although some patients may experience relapse, CAR-T cell therapy offers a more promising prospect for long-term cure compared to conventional chemotherapy regimens for DLBCL patients. Similarly, in the treatment of relapsed/refractory B-ALL, CD19-targeted CAR-T cell therapy can achieve complete response (CR) rates of 70% to 90%. However, unlike DLBCL, the challenges in treating B-ALL with CAR-T cells include higher relapse rates and the occurrence of severe cytokine release syndrome (CRS).
Currently, the duration of overall response maintenance with CAR-T cell therapy is shorter in B-ALL compared to DLBCL. The targets, efficacy, and adverse event profiles of CAR-T cell therapy in MM also differ from those observed in DLBCL and B-ALL.
2. Application of CAR-T in MM Treatment
The correct selection of the target antigen often plays a decisive role in the clinical efficacy of CAR-T therapy. Currently, the main targets are tumor-specific antigens (TSAs) and tumor-associated antigens (TAAs). TSAs are expressed only on tumor cells but not on normal tissue cells, and are very rare. TAAs are highly expressed on tumor cells and have low expression levels on normal tissue cells, making them more abundant than TSAs. A suitable targeting antigen must be tumor cell-specific, meaning highly expressed on tumor cells and rarely expressed on healthy tissue cells, in order to exert specific and effective anti-tumor effects.
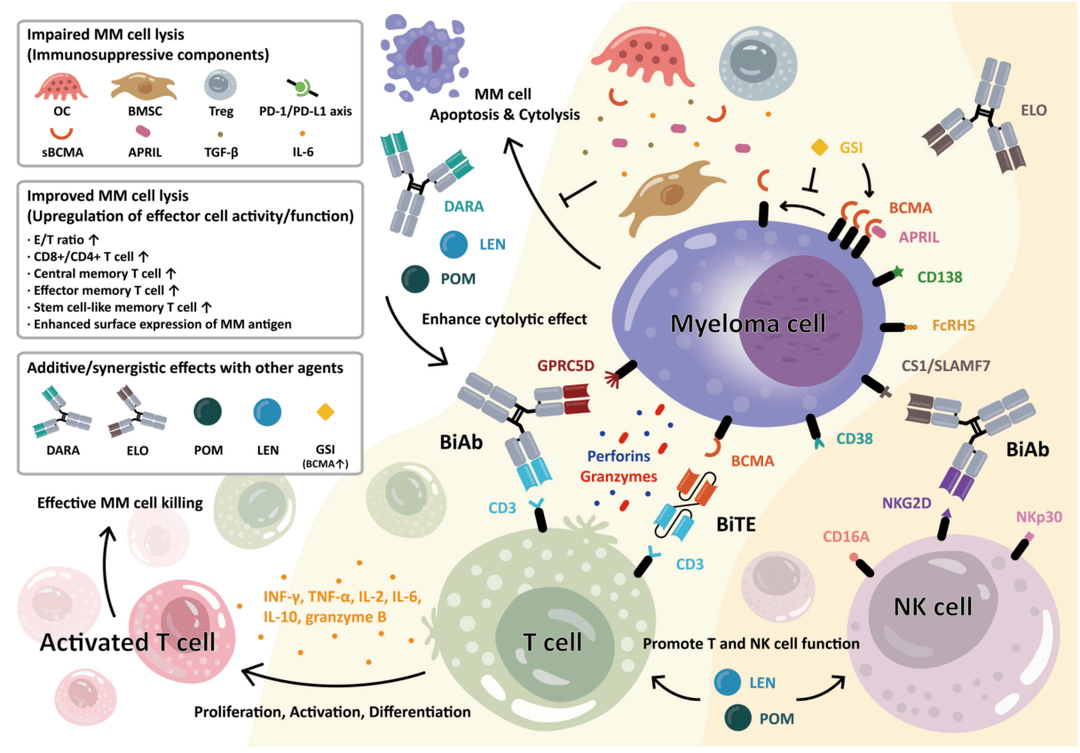
With the development of CAR-T therapy, several targets have been identified for the treatment of MM, including B-cell maturation antigen (BCMA), CD19, CD38, CD138, CD56, signaling lymphocytic activation molecule family 7 (SLAMF7), G protein-coupled receptor family C group 5 member D (GPRC5D), a proliferation-inducing ligand (APRIL), CD267, CD229, CD45, CD44v6, integrin β7, fibronectin 1, Fc receptor homologs 5 (FcRH5), κ-light chain, chemokine C-C-motif receptor 10 (CCR10), and NK cell receptor 2D, among others.
2.1) BCMA
BCMA is currently the most widely used and effective target for CAR-T therapy in MM. BCMA belongs to the TNF receptor superfamily, also known as CD269 or TNF receptor superfamily member 17. BCMA is highly specifically expressed on the surface of plasma cells, with almost no expression on normal cells. Its binding receptors include B-cell activating factor (BAFF) and APRIL. APRIL is mainly produced by bone marrow granulocytes and osteoclasts, and its expression is associated with MM cell proliferation, survival, drug resistance, and immunosuppression. Therefore, BCMA is an ideal target for CAR-T therapy in MM. Currently, BCMA-targeted CAR-T therapy for MM has achieved good efficacy, with an overall response rate of 80-90%.
2.1.1) Single-Target Application of BCMA
In 2016, Ali et al. first demonstrated the efficacy and safety of BCMA-targeted CAR-T cells in the treatment of relapsed/refractory multiple myeloma (RRMM). Subsequently, clinical studies on BCMA-targeted CAR-T therapy reported encouraging results, with response rates over 80%, and even 40-60% of patients achieving minimal residual disease (MRD) negativity. The progression-free survival (PFS) time was 10-14 months, and patients who achieved complete response (CR) or better had a longer PFS.
In March 2021, the US FDA approved the first BCMA-targeted CAR-T product, Ide-cel, for the treatment of adult RRMM patients who had received at least four prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody, and were refractory to these treatments. In the phase I study of Ide-cel, which enrolled 33 RRMM patients, the objective response rate (ORR) was 85%, and the CR rate was 45%. The median PFS for patients who achieved CR was 11.1 months. In the phase II study, which enrolled 128 RRMM patients, the ORR was 73%, the very good partial response (VGPR) rate was 52%, and the CR rate was 33%. The median PFS for patients achieving CR or stringent CR (sCR) was 20.2 months, for those achieving VGPR it was 10.5 months, and for those achieving partial response (PR) it was 4.5 months. In the phase III study, which enrolled 254 RRMM patients, the ORR was 71%, the CR rate was 39%, and the sCR rate was 5%. Eighty-eight percent of patients experienced cytokine release syndrome (CRS), of which 83% were grade 1 or 2. Fifteen percent of patients experienced immune effector cell-associated neurotoxicity syndrome (ICANS), with 12% being grade 1 or 2, and 3% being grade 3 or higher. Ide-cel represents a major breakthrough in the use of BCMA-targeted CAR-T therapy for the treatment of RRMM.
In February 2022, the second BCMA-targeted CAR-T product, Cilta-Cel, was also approved by the US FDA for the treatment of RRMM patients who had received at least four prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody, and were refractory to these treatments. In a single-arm phase Ib/II study of Cilta-Cel, which enrolled 113 RRMM patients, with a median follow-up of 12.4 months, the ORR was 97.9%, the sCR rate was 65%, the 12-month PFS rate was 77%, and the 12-month overall survival rate was 89%, demonstrating the efficacy and safety of this BCMA-targeted CAR-T product. In the B cohort of a phase II, multi-cohort, open-label, multicenter clinical study of Cilta-Cel, with a median follow-up of 10.6 months, the ORR was 95%, the VGPR rate was 90%, the CR rate was 79%, and the 6-month and 12-month PFS rates were 90% and 84%, respectively. Among 13 evaluable patients, 92% showed MRD negativity. Additionally, in a clinical study of Cilta-Cel conducted in eight research centers in China, which enrolled 48 RRMM patients, the ORR was 89.6%, the PFS time to first response was 0.95 months, the 18-month PFS rate was 66.8%, and the 18-month overall survival rate was 78.7%. This study demonstrated that Cilta-Cel can induce early, deep, and durable responses in MM, and may become a treatment option for patients after their first relapse.
There have been reports on the real-world use of the commercialized Ide-cel and Cilta-Cel products. In the United States, 11 institutions used Ide-cel to treat RRMM patients, and the ORR was 84%, with a median PFS of 8.5 months. In a French registry center, 49 RRMM patients were treated with Ide-cel, and the 3-month ORR and PFS rates were 76% and 82%, respectively. Additionally, in 12 US institutions using Cilta-Cel to treat RRMM patients, with a median follow-up of 5.8 months, the best ORR was 89%, and the 6-month PFS rate was 79%. The real-world use results are consistent with clinical studies, but larger sample sizes are needed for further confirmation.
In June 2023, China’s National Medical Products Administration approved the BCMA-targeted CAR-T product Jiejiolun-sai for marketing, for the treatment of adult RRMM patients who had received at least three prior lines of therapy (including at least one proteasome inhibitor and one immunomodulatory agent). This is China’s first domestically developed BCMA-targeted CAR-T product with full production capabilities, and the world’s first CAR-T product containing a fully human single-chain antibody in its CAR structure, unlike previous products with animal-derived CAR structures. This design effectively reduces its immunogenicity in the host while maintaining its anti-tumor activity, and has high safety and efficacy. In the phase I study of Jiejiolun-sai, which enrolled 18 RRMM patients, including 4 patients who had previously received murine-derived CAR-T products targeting BCMA, the ORR was 100%, and 72.2% of patients achieved CR or sCR.
In 2023, the American Society of Clinical Oncology (ASCO) Annual Meeting updated the clinical study results of Iberdomide (IBRD) in treating patients with relapsed/refractory multiple myeloma (RRMM). The results showed: Among the 101 evaluable patients for efficacy, the overall response rate (ORR) was 96.0%, the very good partial response (VGPR) rate was 91.1%, and the complete response (CR) rate was 74.3%. Among the 103 evaluable patients for immunogenicity, only 19.4% of patients were detected with anti-CAR antibodies. In the 89 patients who had not previously received BCMA CAR-T therapy, the ORR was 98.9%, and the CR rate was 78.7%. In the 63 patients with a follow-up of at least 12 months (including those who dropped out before 12 months), the ORR was 98.4%, and the CR rate was 87.3%. These study results demonstrate the excellent safety and efficacy of Iberdomide, showing breakthrough efficacy not only in the overall enrolled population but also in patients who had relapsed after previous CAR-T therapy, indicating a broad application prospect.
In August 2023, The Lancet Oncology updated the clinical study data of ARI0002h, another humanized CAR-T product targeting BCMA. The primary endpoints were the ORR at 100 days post-infusion and the proportion of patients experiencing cytokine release syndrome (CRS) or immune effector cell-associated neurotoxicity syndrome (ICANS) within 30 days of treatment. The researchers adopted a split-dose infusion followed by a boost infusion regimen. The ORR at 100 days post-infusion was 100%, with a CR rate of 67%, a very good CR (VGCR) rate of 27%, and a partial response (PR) rate of 7%. Among the patients who achieved CR, 60% achieved stringent CR (sCR). 80% of patients experienced only grade 1-2 CRS, and no patients experienced ICANS. This study suggests that through the split-dose infusion combined with a boost dose, ARI0002h can induce deep remission in MM patients with poor prognosis while maintaining good safety.
2.1.2) Combination of Multiple BCMA Targets
Although the use of single-target BCMA CAR-T therapy in treating RRMM has achieved encouraging efficacy in China and abroad, for some RRMM patients, single-target BCMA CAR-T therapy remains ineffective, or the disease relapses or progresses after an initial response. Antigen loss and escape are among the main reasons for this phenomenon. Some scholars believe that the combination of multiple targets with CAR-T is the best strategy to overcome tumor antigen heterogeneity and antigen escape, which can improve the response rate and survival of RRMM patients receiving CAR-T therapy to a certain extent. The combination of multiple BCMA targets is being actively explored, mainly through tandem bi-specific CARs, combined CARs, logic-gated CARs, and tri-specific CARs, among others. The antibodies used in combination include CD19, CD38, CD138, CS1, and GPRC5D, and related studies have achieved significant efficacy, becoming an effective way to prevent antigen escape. However, this type of CAR-T cells can be recognized and activated by multiple target antigens, which may cause cytokine storms and excessive killing of normal cells with low antigen expression. Optimizing and improving the combination of multiple BCMA targets with CAR-T will be a direction for future exploration.
2.2) GPRC5D
GPRC5D belongs to the orphan receptor family of G protein-coupled receptors and is a seven-transmembrane protein. A study from the Memorial Sloan Kettering Cancer Center in the United States confirmed the high expression of GPRC5D on the surface of plasma cells in multiple myeloma (MM). The study included 83 MM patients, and 65% of them had GPRC5D expression on plasma cells above the threshold. Moreover, GPRC5D is rarely expressed in normal tissues, except in the immune-privileged hair follicle region, suggesting that GPRC5D can be a therapeutic target for MM. As GPRC5D is a seven-transmembrane protein, it is less likely to undergo antigen loss and is independent of BCMA expression, bringing new hope for MM patients who do not express BCMA. Therefore, GPRC5D is an attractive target for MM treatment. MCARH109 is a CAR-T product targeting GPRC5D, and its phase I clinical trial included 17 RRMM patients, including those who relapsed after BCMA CAR-T therapy. 59% of patients achieved at least a very good partial response (VGPR).
This is the first officially published efficacy data of GPRC5D-targeted CAR-T therapy in RRMM patients. Additionally, the results of a study conducted by Chinese scholars using GPRC5D-targeted CAR-T therapy in RRMM patients also demonstrated similar efficacy, with an ORR of 91% and a sCR rate of 33% among the 33 RRMM patients enrolled. Furthermore, Professor Huang He’s team from the First Affiliated Hospital, Zhejiang University School of Medicine conducted the first single-center, single-arm phase I clinical trial of GPRC5D-targeted CAR-T therapy in RRMM, enrolling 12 RRMM patients. Two patients discontinued treatment due to disease progression, while the remaining 10 patients achieved an ORR of 100%, with a sCR rate of 60% and a VGPR rate of 40%. No severe adverse events such as ICANS were reported in this study.
2.3) FcRH5
FcRH5 is a protein containing an Ig domain and is exclusively expressed in the B-cell lineage. FcRH5 is expressed in nearly 100% of myeloma cells, and its expression level on myeloma cells is higher than that on normal B cells. Recently, a team from the First Affiliated Hospital of Soochow University detected significantly higher expression of the FcRH5 antigen than BCMA in CD138-positive MM patient myeloma cells. They then constructed an FcRH5-targeted CAR-T cell and applied it to a xenograft mouse model, demonstrating potent anti-tumor efficacy. The study also found that different forms of soluble FcRH5 could interfere with the efficacy of FcRH5 CAR-T cells. Additionally, the researchers constructed a bi-specific CAR-T cell targeting both FcRH5 and BCMA, which showed better efficacy in the mouse model compared to the single-specific FcRH5 CAR-T cell.
3. Safety Issues and Strategies in CAR-T Cell Therapy
Safety is a prerequisite for the application of CAR-T cell therapy. Studies that have summarized long-term follow-up data from patients receiving CD19- and BCMA-targeted CAR-T cell therapies have found that CD19-targeted CAR-T cells for the treatment of B-cell malignancies can lead to long-term remission in patients, typically with only low-grade adverse events. In comparison, BCMA-targeted CAR-T cell therapy for multiple myeloma (MM) results in shorter remission durations, although some patients can achieve long-term remission, and low-grade adverse events are generally observed. The favorable efficacy and low-level adverse events within a controllable safety range are crucial factors for the further promotion of CAR-T cell therapy.
Although BCMA-targeted CAR-T cells have not exhibited strong off-tumor toxicity in clinical studies so far, all approved CAR-T cell products have demonstrated varying degrees of adverse events, such as cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS), hypogammaglobulinemia, B-cell regeneration deficiency, and cytopenias. A few fatal adverse events have also been observed. Additionally, factors like antigen loss or escape, off-target effects, decreased T-cell quantity or quality, immune rejection, soluble forms of target antigens blocking CARs, and clinical application management can all contribute to safety issues with CAR-T cell therapy and require further investigation. Particularly for MM, enhancing safety control, optimizing CAR-T cells, and reducing adverse events remain areas in need of improvement.
3.1) Improving CAR-T Cell Toxicity
CRS and ICANS are two adverse events caused by CAR-T cell therapy that require clinical attention. The host immune system’s recognition of CARs may be related to the occurrence of CRS. Therefore, the use of humanized antibody fragments can reduce CAR immunogenicity and mitigate adverse events. Furthermore, reducing the affinity of the CAR-T cell antigen-binding domain, modifying the hinge and transmembrane regions to alter the activation of CAR-T cells, and regulating cytokine secretion can also reduce adverse events. Alternatively, implementing a “CAR-T switch” or suicide gene strategy to selectively reduce CAR-T cell function when adverse events occur are feasible measures to proactively reduce the risk of adverse events. However, ICANS can present in various forms, including encephalopathy, cognitive deficits, language disorders, seizures, and brain edema. Some early ICANS may present as localized neurological symptoms. It is worth noting that even mild ICANS symptoms should be monitored closely, as the condition can rapidly worsen. Therefore, establishing a universal grading and monitoring system for CRS and ICANS is crucial for early detection and treatment.
3.2) Optimizing CAR-T Cell Construction
Antigen loss or escape is a major mechanism of relapse and resistance to CAR-T cell therapy in MM patients and is one of the reasons for its limited efficacy. For some MM patients who initially respond to CAR-T cell therapy, treatment response may be lost, and tumor relapse may occur over time. Long-term antigen exposure can lead to functional exhaustion of CAR-T cells, resulting in the appearance of aged CAR-T cell phenotypes. In such cases, antigen detection may show a lack of antigen expression. Downregulation or loss of BCMA expression has also been observed in MM patients after receiving BCMA-targeted CAR-T cell therapy. Off-target effects are another reason for the limited efficacy of CAR-T cell therapy. The ideal target antigen should be confined to tumor cells, but most CAR-T cell target antigens are also expressed at low levels in normal tissues, potentially leading to adverse events. Therefore, optimizing CAR-T cell construction, reducing antigen loss and escape, and managing off-target effects are areas of focus for researchers. Strategies include using new targets (e.g., BAFF CAR-T cells), developing bi-specific CARs, modifying CAR-T cells with bi-specific T-cell engagers, or using logic-gated CARs.
3.3) Enhancing CAR-T Cell Activity
Decreased T-cell quantity or quality can also limit the efficacy of CAR-T cell therapy. Li et al. used single-cell sequencing to analyze T cells from MM patients who relapsed after BCMA CAR-T cell therapy and found a decrease in the percentage of therapeutic T cells, along with an increase in the percentage of BCMA-positive plasma cells and exhausted T cells. Improving T-cell activity and persistence is crucial for enhancing the efficacy of CAR-T cell therapy. Studies have shown that CAR-T cells containing the 4-1BB costimulatory domain exhibit an enhanced memory T-cell phenotype, which may delay CAR-T cell exhaustion. The combination of T-cell inducible costimulatory molecules and the 4-1BB costimulatory domain in the CAR structure can significantly increase T-cell persistence. Other approaches to improve T-cell persistence include combining CAR-T cells with immune checkpoint inhibitors to enhance T-cell persistence and promote memory T-cell formation, using stem-like T cells, or using CAR-T cells lacking lymphocyte-specific protein tyrosine kinase, all of which can increase T-cell persistence and improve the efficacy of CAR-T cell therapy.
3.4) Quality Control of CAR-T Cells
Currently, there are no uniform quality control standards or consensus for CAR-T cells, but the growing clinical demand for CAR-T cell therapy has brought forth requirements and challenges for quality control. Theoretically, quality control of CAR-T cells should be implemented throughout the various stages of CAR-T cell production. Currently, quality control of CAR-T cells in production primarily focuses on three aspects: safety, potency, and purity. In terms of safety, routine sterile production control, endotoxin, and mycoplasma testing should be performed. If viral vectors are used for CAR-T cell transduction, the quality of the virus needs to be assessed to avoid the risk of replication-competent retroviruses and lentiviruses integrating into the genome. Quality control of CAR-T cell potency primarily refers to the activation state of T cells, typically evaluated by representative indicators (e.g., IFN-γ expression). Quality control of CAR-T cell purity involves the detection of target T cells, non-target cells, and contaminants in the CAR-T cell product, with limits set on the proportions of components other than the target T cells.
3.5) Safety Guidelines for Clinical Application of CAR-T Cell Therapy
Establishing safety guidelines for the clinical application of CAR-T cell therapy is essential for ensuring efficacy and safety. These guidelines should at least include patient screening and baseline evaluation, recommended pre-collection evaluation parameters, selection of bridging therapy, lymphodepleting chemotherapy, CAR-T cell infusion (pre-infusion assessment and infusion management), management of adverse events post-CAR-T cell infusion, and subsequent short- and long-term follow-up.
4. Exploring the Accessibility of CAR-T Cell Therapy
Along with the exciting therapeutic effects and the mushrooming research reports on CAR-T cell therapy, the high cost of this treatment has also become a hot topic of discussion. As of September 2023, nine CAR-T cell therapy products have been approved globally, with three of them receiving approval from the National Medical Products Administration of China. Although the recently launched Yescarta has a slightly lower official price compared to previous products, it remains prohibitively expensive for ordinary patients. Reducing the cost of CAR-T cell products is still a direction that researchers are striving for, with the hope of making CAR-T cell therapy more accessible to a broader patient population in the near future.
4.1) Complexity and Time-Consuming Nature of Traditional CAR-T Cell Preparation
The preparation process for traditional CAR-T cell therapy is complex and lengthy, with a total cycle time of 3-4 weeks. First, peripheral blood mononuclear cells are collected from the patient (or an allogeneic donor) through leukapheresis, and specific T cells are isolated and activated. These T cells are then transduced with a CAR gene using a vector, resulting in the generation of CAR-T cells. The T cell transduction process requires a vector, typically a viral vector, which involves steps such as viral vector construction, T cell transduction with the viral vector, T cell integration, and T cell expression. For multiple myeloma (MM) patients, especially those who have relapsed after multiple lines of treatment, life-threatening situations like tumor progression may occur during this waiting period. Therefore, the long wait time may cause patients to miss the optimal treatment window, highlighting the need to further optimize the CAR-T cell preparation process to shorten the preparation time.
4.2) Novel Methods for CAR-T Cell Preparation
The complex and lengthy production process of CAR-T cells has led to the high cost and limited supply of CAR-T cell therapy. Currently, researchers are developing new preparation methods by exploring alternative vectors, T cell modifications, and T cell sources.
4.2.1) Vector Selection
(1) Nanoparticle technology: The Stephan team employed a biodegradable nanoparticle technology to reprogram immune cells in the body, converting them into CAR-T cells, with the entire process completed within 24-48 hours.
(2) Lentiviral vector expressing infrared fluorescent protein: The Michael team used this vector to prepare functional, antigen-specific CAR-T cells within 24 hours.
(3) Transposon vectors: Wong et al. used the TcBuster transposon system to prepare BAFF CAR-T cells, reducing the preparation time to 7-10 days.
(4) mRNA vectors: The CAR gene is transcribed into mRNA in vitro and then introduced into T cells through electroporation. T cell activation is not required, and CAR-T cells can be prepared within 1 day.
(5) Gene editing for CAR integration: Zhang et al. employed gene editing technology to site-specifically integrate a non-viral PD1 CAR, with CAR-T cell preparation completed in as little as 3 days.
(6) Bioscaffolds: Agarwalla et al. used an implantable multifunctional alginate scaffold to rapidly generate CAR-T cells in vivo, reducing the preparation time to 1 day. Zhang et al. used an antigen-presenting cell scaffold, increasing the expansion efficiency of mouse and human primary T cells by 2-10 fold.
4.2.2) T Cell Modifications
Currently, many new technology platforms are emerging for rapid CAR-T cell preparation through T cell modifications, including the FasT-CAR platform, T-Charge platform, and InstanCAR-T platform.
(1) FasT-CAR platform: This platform combines the three main production steps of “activation, transduction, and expansion” for autologous CAR-T cells into two steps: “synchronous activation-transduction,” significantly reducing the preparation time. GC012F, a bispecific CAR-T product targeting BCMA and CD19, was developed on this platform and can be prepared within 22-36 hours.
(2) T-Charge platform: By preserving the stem-like properties of T cells, the expansion of CAR-T cells primarily occurs in vivo, shortening the ex vivo culture time. PHE885, a BCMA-targeted CAR-T product developed on this platform, reduces the ex vivo culture time to approximately 24 hours.
(3) InstanCAR-T platform: This platform improves the processes of T cell selection, activation, and formulation, reducing the need for ex vivo expansion steps.
4.2.3) Changes in T Cell Sources
Traditional CAR-T cells are derived from the patient’s own T cells, while UCAR-T (Universal CAR-T) cells are derived from healthy donors. UCAR-T, also known as allogeneic CAR-T or off-the-shelf CAR-T, involves isolating T cells from healthy donors, modifying them, and expanding them ex vivo, after which they can be administered to multiple patients without the need for the lengthy preparation of autologous CAR-T cells. UCAR-T enables scalable and standardized production processes, potentially reducing production costs by up to 90%. ALLO-715 is the first UCAR-T product for the treatment of relapsed/refractory multiple myeloma (RRMM). It targets BCMA and employs gene editing techniques to knock out the T cell receptor alpha chain and CD52 antigen, reducing the risk of graft-versus-host disease mediated by the T cell receptor and improving CAR-T cell engraftment. Phase I clinical trial results for ALLO-715 showed an overall response rate (ORR) of 70.8%, a very good partial response (VGPR) rate of 45.8%, and a complete response (CR) rate of 25%. Additionally, 55.8% of patients experienced grade 3 or lower cytokine release syndrome (CRS), and 14% experienced grade 3 or lower immune effector cell-associated neurotoxicity syndrome (ICANS). These preliminary results support the feasibility and safety of UCAR-T cell therapy for MM.
5. Summary and Outlook
In recent years, the treatment of MM has undergone significant and transformative advancements, with cellular immunotherapy becoming the new driving force in MM treatment. As a novel therapeutic modality with a unique mechanism of action, CAR-T cell therapy has brought hope for treatment or even cure to patients with RRMM. An increasing number of CAR-T products are entering the new drug research stage. How to better translate CAR-T cell therapy into survival benefits for patients, how to further optimize and improve CAR-T cells to enhance therapeutic efficacy while reducing adverse events, and how to make CAR-T cell therapy more accessible and economically viable – these are all areas that require in-depth research and discussion.
Content source:中华移植
